When the Clock Stops, the Chaos Creeps In
I didn’t expect it to feel like this.
After 90 days in treatment, I had structure. I had a morning routine. I had people. I had accountability. I knew what was expected of me, and for the first time in a long time, I met it. But when I stepped out—bags packed, discharge papers in hand—it was like the air changed. Time slowed down, and so did I.
No more wake-up calls. No more groups. No more head-nods from the guy who always saved me a seat.
And the quiet got loud.
The truth is, no one really prepares you for what happens when the structure of a residential treatment program disappears. Not because they don’t care. But because some things can’t be simulated. You have to live through the weirdness of it to understand it.
Structure Wasn’t Control. It Was Support.
During treatment, I used to get annoyed at the schedule. I rolled my eyes at morning meditation. I dragged my feet to groups. I thought: When I’m out of here, I’m doing things my way.
But looking back, that structure was more than a routine—it was my recovery’s backbone. It gave my body and brain the message: You’re safe now. You can rest. You can grow.
It wasn’t about control. It was a container. A container that held my pain, my confusion, and my potential all at once.
So when I left and that container disappeared, everything spilled out.
Relapse Doesn’t Erase Progress—It Signals a Need
It took just three weeks.
Three weeks before I found myself driving to a liquor store. Not because I wanted to drink—but because I didn’t know what else to do with the ache in my chest. The people I called didn’t answer. The routine I said I’d follow was gone by day four. My body felt loose, like a marionette without strings.
I drank. And instantly regretted it.
That moment broke me—but not in the way you might think. It broke the illusion that I could “do this solo.” That I didn’t need anyone. That 90 days had made me immune to old pain.
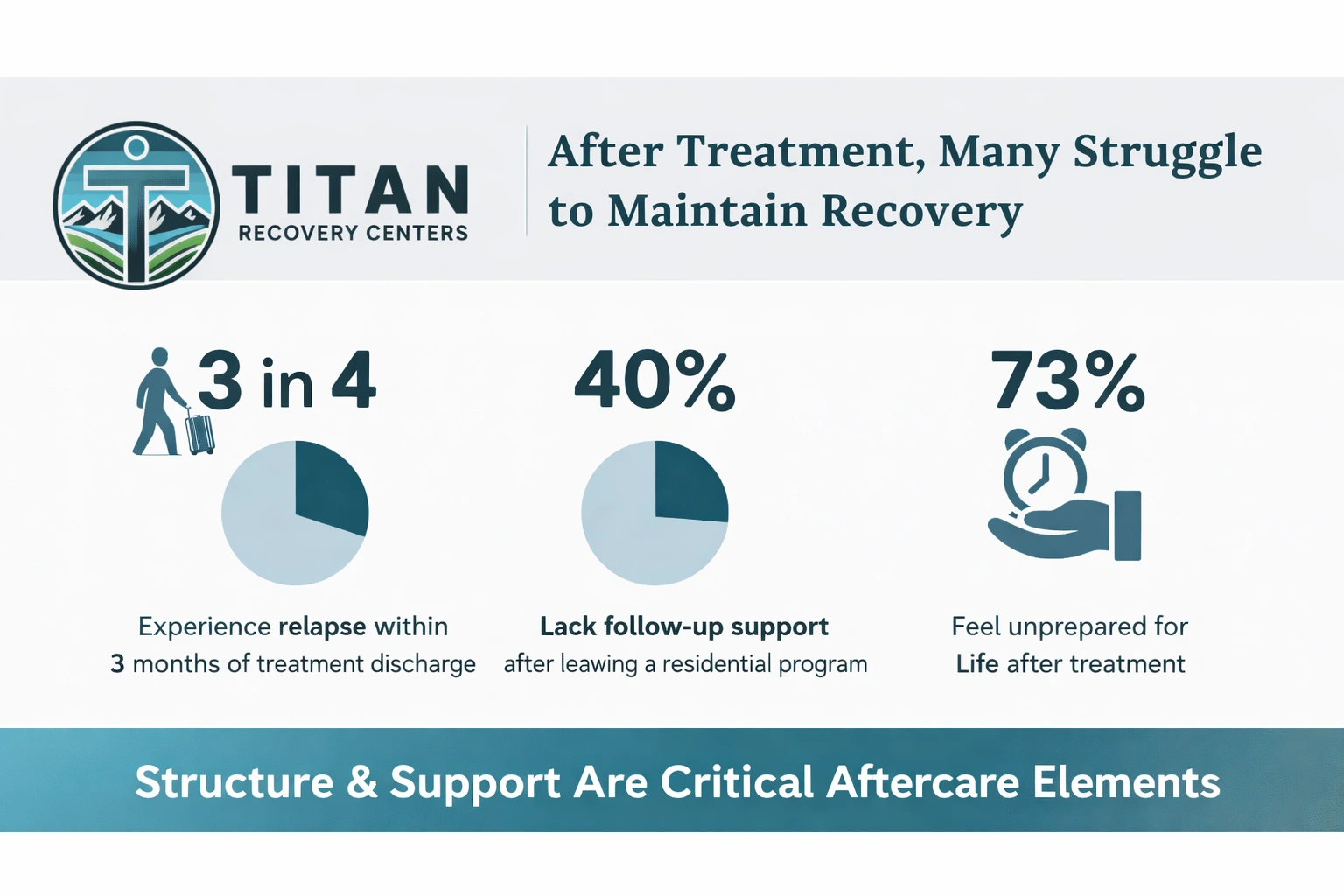
If you’ve been there—if you’ve relapsed after time in a residential treatment program—please hear me: it doesn’t mean you failed. It means something was missing. And most of the time, that something is connection, support, or structure—not willpower.
Why Discharge Can Feel Like Free Fall
There’s something nobody warns you about: when you leave a treatment center, the world doesn’t stop for your transition.
Your job expects you back. Family dynamics resurface. Bills pile up. And somehow, you’re supposed to remember how to be a person in all that chaos.
It’s not just overwhelming—it’s disorienting.
In treatment, your world narrows in a healing way. You focus inward. You rewire. But when that world expands again post-discharge, you don’t have a built-in guidebook.
And if you haven’t built aftercare supports—like therapy, alumni groups, outpatient care—that sudden expansion can feel like free fall.
How to Rebuild Structure Without Feeling Like You’re “Back in Rehab”
Here’s something I wish I had known: you don’t have to recreate the exact structure of your residential program to feel safe again.
You just need anchors. Predictability. Safe people. Healthy repetition.
Try this:
- Bookend your day. Morning routines and nighttime wind-downs give your body a rhythm again.
- Add just one thing each day that’s “for” your recovery. That could be journaling, calling a sober friend, or reading a meditation.
- Revisit your treatment materials. Look at the notes, mantras, or worksheets you once found helpful. They’re not locked in a past chapter—you can reuse them now.
- Name your lifelines. Make a list of 3–5 people you can text when things start to wobble—even if you don’t know what to say.
This isn’t about going backwards. It’s about giving yourself scaffolding to grow in new soil.
Alumni Slump Is Real—And It’s Not Just You
There’s a quiet truth a lot of alumni carry: once the confetti of graduation fades, it can feel lonely.
The people who were in your daily life in treatment are now scattered across states. The support staff you saw every morning? You might not talk to them again. Even your own family might not understand how strange and shaky the transition feels.
That “alumni slump” can show up as:
- Feeling disconnected, even when you’re around people
- Wondering if you’re still “doing recovery right”
- Comparing yourself to others who “seem to be thriving”
- Slipping into habits of isolation or silence
But it’s not permanent. It’s not proof you’re broken. It’s just a part of recovery that’s rarely talked about.
What to Do If You Feel Yourself Slipping
If you feel off, don’t wait until you’re in a crisis to speak up.
Early warning signs are sacred. They’re your body and mind waving a gentle flag that says, I need something different. Not something drastic—just different.
You might need:
- A phone call with someone from your program
- A week back in a structured setting
- To attend a group again, even if it’s been a while
- A change in environment or schedule
And if you’re near Vegas or looking for a residential treatment program in North Las Vegas, know that Titan Recovery welcomes alumni with open arms. Not judgment. Not shame.
Coming Back Isn’t Going Backward—It’s Choosing to Keep Going
Some people think returning to care means they’ve “lost their progress.” That couldn’t be further from the truth.
Coming back says:
- I’m worth continuing to fight for.
- I remember what stability felt like, and I want it again.
- I trust myself enough to ask for help before I unravel.
You’re not starting over. You’re restarting from experience. And that makes all the difference.
Even if you’re not sure you “need” residential again, reconnecting to a structured program—even briefly—can be a reset. It can be the moment your body remembers what safety felt like.
If you’re in the Vegas area and looking for help for people in Henderson, NV, Titan offers personalized support that meets you where you are now—not where you think you “should” be.
FAQs About Life After Residential Treatment
How long does the “adjustment period” last after leaving residential care?
It varies, but many people report the first 30–90 days post-discharge feel the most unstable. That doesn’t mean it’s all downhill—just that your nervous system is still recalibrating. Give yourself grace and structure during this phase.
Is it normal to relapse after completing a residential treatment program?
Yes. While not inevitable, relapse is a common experience in recovery—and it’s not a moral failure. It signals a need for more or different support. The most important thing is to respond quickly and compassionately.
Do I have to go back to residential treatment if I relapse?
Not always. Some people benefit from a return to residential care, especially if their environment is unsafe. Others stabilize through outpatient care, peer support, or structured routines. The right choice depends on your unique situation.
What if I miss the connection I had during treatment?
That’s a real and valid ache. You can rebuild connection through alumni groups, sober communities, or even re-engaging with your former treatment center. Recovery isn’t meant to be lonely—don’t be afraid to reach out.
Can I re-enter treatment if I already “graduated”?
Absolutely. Recovery is lifelong. Titan Recovery Centers welcomes alumni who need another round of care—without shame, without judgment. You’re always welcome back.
You’re Not Broken—You’re Just Between Structures
If you’re out of treatment and feel like the ground beneath you is shifting, you’re not broken. You’re in transition. And transition is tender.
You don’t have to “start over.” You don’t have to hide. You just have to take one small action—today—that reconnects you to support.
That might be a phone call. A message. A return visit. A breath.
And if you’re near Las Vegas and ready to reconnect, call (888) 976-8457 or visit Titan Recovery’s Residential Treatment Program to explore your next step.




